Что такое нейропатическая боль?
Нейропатическая боль — это вид боли, который, в отличие от обычной боли, возникает не вследствие реакции на физическое повреждение, а в результате патологического возбуждения нейронов в периферической или центральной нервной системе, отвечающих за реакцию на физическое повреждение организма (обычную боль).
Нейропатическая боль может быть ассоциирована с аномальными ощущениями (дизестезия) или болью, вызываемой стимулами, которые в норме не вызывают боли (аллодиния). Она может быть постоянной и / или эпизодической. Последняя бывает пронзающей или похожей на удары электрическим током. Общие качества включают жжение или холод, ощущения мурашек и иголок, онемение и зуд. Причиной нейропатической боли могут быть патологические процессы в периферической и центральной нервной системе. Таким образом, различают периферическую нейропатию, нейропатическую боль центрального и смешанного генеза. Нейропатическая боль поражает 7–8% населения Европы, а у 5% людей она может быть тяжелой.
Клинические проявления
 Нейропатические боли, как правило, имеют хроническое течение.
Нейропатические боли, как правило, имеют хроническое течение.
Для субъективной характеристики НБ больные используют такие определения, как жгучая, колющая, стреляющая, режущая. Для этих болей характерен комплекс специфических сенсорных расстройств, которые можно разделить на две группы. С одной стороны, это позитивные спонтанные (спонтанная боль, дизестезии, парестезии) и вызванные (аллодиния, гипералгезия, гиперестезия, гиперпатия) симптомы, с другой – негативные (гипестезия, гипалгезия) симптомы выпадения функции поврежденных структур. Для НБ характерна комбинация позитивных и негативных симптомов, меняющаяся у одного и того же больного в течение заболевания.
Очень характерным для нейропатического вида боли является феномен аллодинии – появление боли в ответ на стимул, который у здоровых людей ее не вызывает. В таких случаях больные испытывают сильные боли при малейшем прикосновении, иногда даже при дуновении ветра.
Различают температурную и механическую аллодинию. Механическая подразделяется на статическую, которая появляется при давлении на фиксированную точку кожного покрова, и динамическую, возникающую при движущихся стимулах (раздражение кожи кисточкой или пальцем).
При гипералгезии чувствительность к болевому стимулу оказывается значительно выше, чем ожидается в норме. При гиперпатии субъективный ответ как на болевой, так и на неболевой стимулы является чрезмерным и часто сохраняется в течение долгого времени после прекращения раздражения. Чувства щекотания, безболезненного покалывания и другие подобные ощущения относятся к парестезиям; если эти ощущения причиняют боль, их называют дизестезиями. Типичный пример НБ – феномен невралгии (тригеминальная, постгерпетическая). Одним из характерных симптомов НБ является каузалгия – интенсивная упорная жгучая боль, нередко носящая ланцинирующий характер, сочетающаяся с аллодинией и гиперпатией и часто сопровождающаяся сосудистыми и трофическими нарушениями. Сочетание жгучей боли с выраженными трофическими расстройствами, а также эффективность в части случаев симпатических блокад послужили поводом для предположения об участии в формировании этой боли симпатической нервной системы. Такую боль называют также симпатически поддерживаемой болью.
Клиническими признаками НБ являются
- отсутствие причины для прямого раздражения ноцицепторов на периферии (травмы, воспаления, ишемии);
- персистирующий, длительный характер боли;
- неэффективность анальгетиков для купирования боли;
- локализация боли в зоне сенсорного дефекта, соответствующего поражению какого-либо отдела нервной системы;
- наличие стимулозависимых болевых феноменов – аллодинии, гипералгезии, гиперестезии, гиперпатии;
- сочетание с вегетативными расстройствами в области боли в виде снижения кровотока, гипер- или гипогидроза и т.д.;
- сочетание с моторными расстройствами;
- частое ухудшение самочувствия по ночам.
В жалобах пациентов патогномоничными дескрипторами боли считаются следующие определения: жгучая, стреляющая, дергающая, режущая или сравнимая с ощущением прохождения электрического тока.
Для НБ характерны коморбидные расстройства, в частности, нарушения сна, расстройства настроения в виде симптомов депрессии и тревоги. Распространенность депрессивных и тревожных расстройств у пациентов с НБ значительно выше, чем в общей популяции. У больных с сочетанием хронической боли и депрессии качество жизни хуже, а интенсивность боли выше. Тревога также является частым коморбидным состоянием при НБ. Пациенты с хронической болью обычно испытывают тревогу как результат стресса от жизни с болью. Боль может вызывать изменения уровня тревоги, а повышенная тревога способна усилить восприятие боли.
Причины
 Нейропатическая боль центрального генеза наблюдается при повреждениях спинного мозга, рассеянном склерозе, иногда при инсультах. Кроме диабета, самыми частыми причинами болей при периферической нейропатии являются герпесвирусная инфекция, ВИЧ-ассоциированная нейропатия, недостаток некоторых питательных веществ, действие токсинов, паранеопластический синдром, расстройства иммунной системы, травмы нервных стволов. Периферическая полинейропатия - самый частый симптом при болезни Фабри.
Нейропатическая боль центрального генеза наблюдается при повреждениях спинного мозга, рассеянном склерозе, иногда при инсультах. Кроме диабета, самыми частыми причинами болей при периферической нейропатии являются герпесвирусная инфекция, ВИЧ-ассоциированная нейропатия, недостаток некоторых питательных веществ, действие токсинов, паранеопластический синдром, расстройства иммунной системы, травмы нервных стволов. Периферическая полинейропатия - самый частый симптом при болезни Фабри.
Нейропатическая боль часто встречается при онкологических заболеваниях; она вызывается прямым воздействием опухоли на периферические нервы (например, путём сдавления) или как побочный эффект химиотерапии, лучевой терапии или хирургического вмешательства.
Характерные ощущения при нейропатической боли
- Онемение
- Жжение
- Покалывание
- Прохождение электрического тока
- Стреляющие боли
- «Ползание мурашек»
Эти боли встречаются часто
Мы все знакомы с болью – будь то головная, зубная боль или боль в мышцах после физической нагрузки. Но есть совсем другая боль, которая связана с поражением нервов. Именно она зачастую становится мучительной, нарушает жизнь человека на протяжении многих месяцев или лет. Эту боль принято называть нейропатической.
.. Мне казалось глупым идти на прием к врачу по поводу онемения в стопах. Хотелось бы знать раньше, что это оказывается нейропатическая боль и ее можно лечить..
Она встречается у 6-7 из 100 человек. Нейропатическая боль может сделать выполнение даже самых элементарных действий, таких как, одеть носки, сорочку, прогуляться, невозможным. Зачастую люди не понимают, что это за боль и как рассказать о ней врачу. Они не могут найти слова для ее описания. Поэтому нередко эти пациенты не получают должной помощи и нужного лечения.
Как возникает нейропатическая боль
У нас в организме существуют миллионы нервов, взаимодействующих друг с другом. Все вместе они образуют нервную систему. Представьте себе множество электрических и телефонных проводов соединяющих Ваш мозг с различными участками тела. Например, когда вы ступаете на пляже на горячий песок, нервы, расположенные на стопе, посылают сигнал в мозг, сообщающий о том, что Вы наступаете на что-то горячее. В результате, Вы чувствуете в стопе жжение. Или, если Вы случайно дотронулись до оголенного электрического провода, то нервы на руке отправляют в мозг быстрый сигнал о том, что Вас ударило током.
Но если происходит повреждение нервов, они начинают работать неправильно и посылают неверные сигналы в мозг. Так, например, поврежденные нервы могут сообщать мозгу о том, что Вы наступили на горячее или дотронулись до электрического провода. И это при том, что на самом деле Вы ни на что не наступали и ничего не трогали. Нервы могут оказаться поврежденными в результате многих причин, таких как, сахарный диабет, герпесная инфекция, травмы рук и ног, нарушения в позвоночнике, инсульты, онкологические заболевания и др.
Нейропатическая боль это как…
Многие люди, имеющие нейропатическую боль, часто не описывают свои ощущения как боль. Напротив, они могут рассказывать о том, что ощущают «множество иголок, заноз», «мурашки», покалывание, онемение, чувствуют «прохождение электрического тока».
... Я чувствовал, что иду как по битому стеклу ...
... Как будто мне вводят в ногу горячую иглу ...
... У меня под кожей тысяча заноз ...
Очень часто боль может быть вызвана чем-то, что в обычных условиях не вызывает боли: прикосновением одеждой, простыней, одеялом и т.д. Иногда боль может быть спонтанной и очень сильной. Но проблема в том, что она «невидима». В отличие от травмы или артрита Вы не видите ее причину, и трудно понять - с чем она связана.
Нейропатическая боль нарушает повседневную жизнь
Если нейропатическая боль лечится неправильно, это может привести к существенному нарушению повседневной жизни. Обычная прогулка в магазин может стать мучением. Даже процесс одевания или ношения одежды, прикосновение постельного белья может сопровождаться выраженными жгучими болями.
... Я ничего не могу делать, не испытывая боль. Я не сплю. Никто в моей семье не знает через какие страдания я прохожу каждый день ...
Многие люди, страдающие нейропатической болью, не могут хорошо спать и не способны работать. Они перестают верить в избавление от этих болей, теряют надежду и становятся депрессивными. Они предпочитают не выходить из дома, меньше общаются с членами семьи и друзьями.
Наиболее частые варианты нейропатической боли
Нейропатическая боль, обусловленная диабетическим поражением нервов
Поражение нервов при диабете называют диабетической полиневропатией. Особенно часто она развивается при высоком содержании глюкозы в крови. Почти у половины больных с диабетической полиневропатией бывают нейропатические боли, которые включают:
- покалывание в стопах, пальцах стоп
- жжение в стопах, усиливающееся ночью
- боль при ношении обуви и/или стоянии и ходьбе
Нейропатическая боль, обусловленная герпесной инфекцией
Боль, возникающая после опоясывающего герпеса, называется постгерпетической невралгией. Она развивается чаще у пожилых лиц после исчезновения характерной сыпи. Может длиться 3 и более месяцев и характеризуется:
- жгучими болями в зоне, где были высыпания
- болями при прикосновении одежды, постельного белья
- длительным течением, нарушением сна
Нейропатическая боль после травмы спинного мозга
После травмы спинного мозга пациентов могут беспокоить сильные боли. Часто они связаны с повреждением нервов, проходящих в спинном мозге, и относятся к нейропатическому типу боли. Это жгучие, колющие, стреляющие болевые ощущения в руках, ногах, туловище, иногда очень сильные.
Нейропатическая боль после инсульта
Примерно у 8% больных, перенесших мозговой инсульт, через некоторое время (от 1 месяца до 2 лет) на больной стороне, или в руке и/или ноге, могут появиться неприятные ощущения в виде покалывания, жжения, боли при контакте с холодными предметами, «рука мерзнет». Поэтому, чтобы уменьшить боль некоторые пациенты носят варежку. Этот тип нейропатической боли называется постинсультная центральная боль. Ее причиной является поражение нервов в области головного мозга.
Нейропатическая боль после хирургических операций
После хирургических операций некоторых больных длительное время беспокоят боли и неприятные ощущения жжения, покалывания, «мурашек» в зоне постоперационного шва. Это связано с частичным повреждением периферических нервов в области хирургического вмешательства. Такие нейропатические боли нередко возникают после операций по удалению молочной железы (мастэктомии) и др.
Нейропатическая боль в спине
У каждого из нас, так или иначе, иногда болит спина. Чаще это связано с напряжением мышц, изменениями в суставах позвонков. Но если происходит сдавление выходящих из позвоночника нервных корешков (например, грыжей межпозвоночного диска), то может возникнуть нейропатическая боль: острые простреливающие боли от поясницы до пальцев стопы, в сочетании с ощущением жжения , покалывания и онемения в ноге. Иногда эти боли быстро проходят, но у некоторых больных могут сохраняться длительное время и не поддаются обычным методам обезболивания.
Нейропатическая боль в лице
Нейропатическая боль может возникать в виде приступов. Например, у некоторых людей старшего и пожилого возраста во время разговора, принятия пищи или при прикосновении к лицу возникают приступы сильнейших болей в половине лица. Это связано со сдавлением тройничного нерва, который отвечает за чувствительность в области лица. Причиной сдавления чаще всего является расположенный рядом кровеносный сосуд. Это заболевание называют невралгией тройничного нерва. Приступы боли очень мучительны, могут продолжаться годами, нарушают работоспособность человека.
Сделайте первый шаг к избавлению от боли
Существуют разные способы лечения нейропатической боли. Но при этом Вы должны активно участвовать в процессе лечения и быть наряду с врачом ответственным за его результаты. Уже половина дела будет сделана, если Вы будете активны и начнете помогать себе.
Что для этого нужно сделать ?
► Расскажите своему врачу о боли и обсудите - какое лечение для Вас будет наилучшим.
► Узнайте, какие есть специальные лекарства для лечения именно нейропатической боли.
► Постарайтесь обговорить с врачом все аспекты предстоящего лечения: длительность, эффективность, сочетание препаратов, побочные явления и т.д.
► Продумайте для себя возможность выполнения программы умеренных физических упражнений.
► Постарайтесь овладеть методиками релаксации.
► Попросите членов семьи, друзей помогать Вам в процессе лечения.
Лечение
В лечении используется комплексный подход – психотерапия, физиотерапия и фармакотерапия.
В фармакотерапии в первую очередь применяются антиконвульсанты (габапентин (Нейронтин), прегабалин (Лирика), классические трициклические (амитриптилин), так и более новые - ингибиторы обратного захвата норадреналина и серотонина (дулоксетин, венлафаксин).
Для устранения периферических болей рекомендуют лидокаин в виде кремов или пластин (Версатис). Курс лечения зависит от клинической формы и может варьировать от 1 до 6 месяцев.
Таким образом, лечение нейропатической боли в настоящее время остается сложной задачей. Представленные выше принципы и алгоритмы лечения могут помочь врачу проводить наиболее эффективное и безопасное лечение пациентов с нейропатическим болевым синдромом. В будущем успех и перспективы лечения связывают с разработкой препаратов, воздействующих на конкретные патофизиологические механизмы данного синдрома.
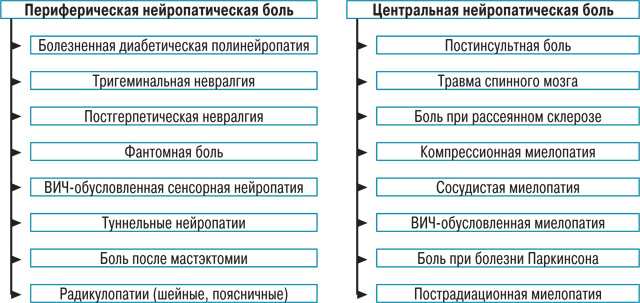
Нейропатическая боль – это болевой синдром, обусловленный поражением соматосенсорной нервной системы вследствие самых разных причин, смотри Таблицу 1.
Наиболее признанной в лечении нейропатической боли на сегодняшний день является фармакотерапия. Основные препараты и их характеристики приведены в Таблице 2.
В Таблице 3 приведены рекомендации Европейской федерации неврологических обществ (EFNS) по терапии некоторых состояний, сопровождающихся нейропатической болью. Эксперты этой федерации провели анализ всех клинических исследований по нейропатической боли, зарегистрированных в Кокрановской библиотеке (база данных доказательных клинических исследований), начиная с 1966 года. В результате были отобраны исследования с высоким уровнем доказательности, и на их основании построены европейские рекомендации по фармакотерапии.
На сегодняшний день неизвестно, является ли неэффективность одного препарата предиктором неэффективности другого или всей последующей медикаментозной терапии. В том случае, если первый назначенный препарат оказался малоэффективным или плохо переносился пациентом, следует переключаться на альтернативную монотерапию препаратом первого ряда (рис. 1). Если все препараты первого ряда оказались неэффективными или плохо переносимыми, то рекомендуется начать монотерапию трамадолом или его комбинацией с парацетамолом либо опиоидным анальгетиком. К сожалению, это не всегда возможно, так как назначение опиоидных препаратов ограничено специальными требованиями, предъявляемыми к выписке этих препаратов.
Анализ болевого синдрома с точки зрения его патофизиологических механизмов (ноцицептивная, нейропатическая, смешанная) оказался очень важным прежде всего с точки зрения лечения. Если врач оценивает боль как ноцицептивную, то наилучшими средствами для ее лечения будут простые анальгетики и НПВП. Если боль является нейропатической или имеется нейропатический компонент, то препаратами выбора являются антиконвульсанты (прегабалин), антидепрессанты, опиоидные анальгетики и лидокаин, особенности которых обсуждались выше (рис. 2).
В случае смешанных болевых синдромов, возможна комбинированная терапия с выбором средств в зависимости от представленности ноцицептивного и нейропатического компонентов (рис. 3).
Via adanilov.ru & rmj.ru & wiki
Created/Updated: 25.05.2018
